Understanding the External Review Process
The Health Carrier External Review Act provides standards for the establishment and maintenance of external review procedures to assure covered persons have the opportunity for an independent review of an adverse benefit determination or final adverse benefit determination.
Commonly Asked Questions
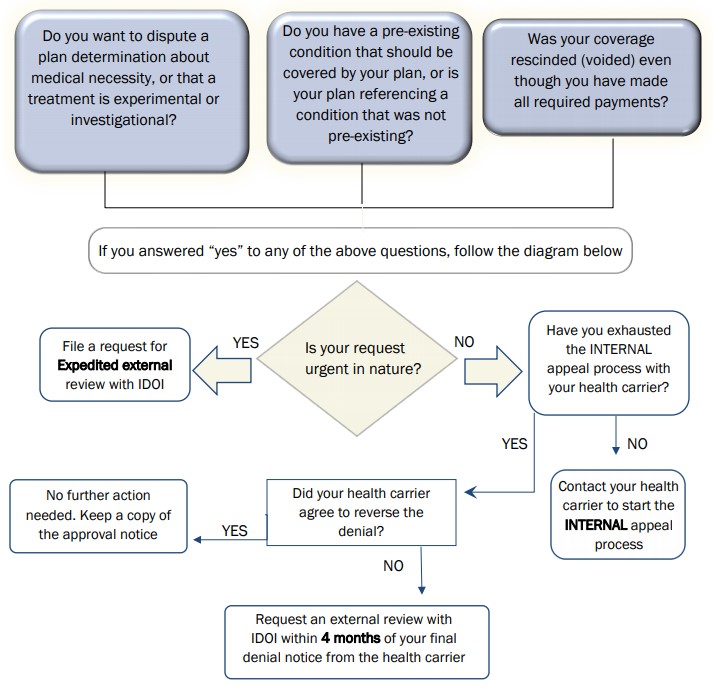
Is my denial eligible for external review? Denials that involve medical judgment, determination of experimental or investigational treatment, pre-existing conditions, or rescission of coverage for a reason other than nonpayment of premium or contributions are eligible for external review. The above includes, but is not limited to, medical necessity, appropriateness, effectiveness of a benefit, level of care, healthcare setting, length of treatment.
Why should I request an external review? When your health carrier denies medical care or treatment, they are required by law to provide a process to appeal the denial. If you complete your health carrier's internal appeal process and your request is still denied, you may be eligible for an external review. An external review is an independent medical review of a health carrier's decision conducted by an Independent Review Organization (IRO) that is approved by IDOI. In Illinois there is no cost to the consumer to file an external review. Note: Illinois Law Commonly Asked Questions 2 of 3.
When can I file an external review? You must file your external review within 4 months of receipt of your final adverse benefit determination (denial) from the health carrier.
What if my situation is urgent, or experimental or investigational? Your health care provider will need to complete the applicable certification form and submit to IDOI. Internal appeal and external review rights are exhausted at the same time in expedited circumstances.
What happens if I don't qualify? The Department will notify you that your request for external review has been denied, and when appropriate, information on how to file a complaint with the Department will be provided. If the Department's complaint investigation determines that clinical judgment was utilized, you will be notified of your right to file an external review.
Are all plans subject to the Illinois Health Carrier External Review Act? Not all health plans fall under the jurisdiction of the IDOI. Health plans that may be referred to a separate entity may include the following:
- You are covered by a self-insured employer, union, church, or non-federal governmental plan. Refer to your benefit booklet for appeals process.
- You are covered by a group plan issued in another state.
- The coverage is through Medicare, Medicaid, Federal Employees Health Benefits Program, Tricare or other military coverage.
- The coverage is for a specified disease (for example, "Cancer only"); specified accident or accident only coverage, credit, dental, disability income, hospital indemnity, long-term care insurance, vision care, or other limited supplemental benefits.
IDOI accepts external review requests: Send only copies. Keep your originals.
Online through IDOI Message Center
Email at DOI.externalreview@Illinois.gov
Fax at (217) 557-8495
Mail to 320 W. Washington Street, Springfield, IL 62767